In February we took a short glimpse of the different scientific techniques that are used to create replacement organs. It goes without saying that all of the mentioned ones, 3D bioprinting, Xenotransplantation, stem cell research are fantastic and unique – but for drug discovery research, we have to add lab-on-a-chip technologies as well to the list of the most impressive scientific methods!
This month, we would like to grab the opportunity to guide you through the fascinating story of lab-on-a-chip technologies. But why would we need to talk about it? What is the purpose of the organs-on-chips (OOC) technologies?
The 20th century was often said to be the age of “bio” and we have to admit that since the discovery of the DNA double helix, we live in the age of genetics. With the rapidly evolving sequencing technologies and plummeting costs of sequencing, we have more data than ever before and are learning more and more about our genome, our body and our diseases. Personalised medicine was born with the help of the information that is provided by “omics” and genetics… and personalised medicine requires new technologies that could support the emerging number of medical test that have to be carried out for the patients.
As we know from our discussions on HLA, everybody is different. When every different patient needs every different existing drug to be tested to find the most personalised solution, a quick, cheap and high-throughput method comes very handy. And this is the point where we need to talk about OOC.
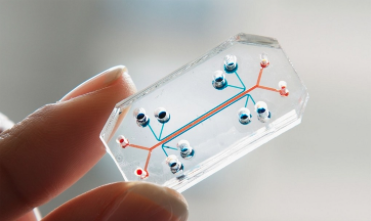
Let’s start from the basics: organs-on-chips is a small microfluidic cell culture device that simulates the function, activities and mechanics of a human organ or organ systems. The OOC has emerged from the lab-on-a-chip devices that integrates different laboratory functions on the surface of one chip.
With the help of the bioprinting technologies, bioengineers are able to use biological inks to print a functioning 3D cellular structures into the microfluidic channels of the microchips. Until 2017, different organs and tissues have been successfully simulated with the microfluidic OOC devices:
A pioneer in the field of OOC research is the Wyss Institute from the Harvard University. Currently they have more than 12 different types of OOC technologies and 1,578 publications in various topics from the world of “Engineering inspired by Biology”.
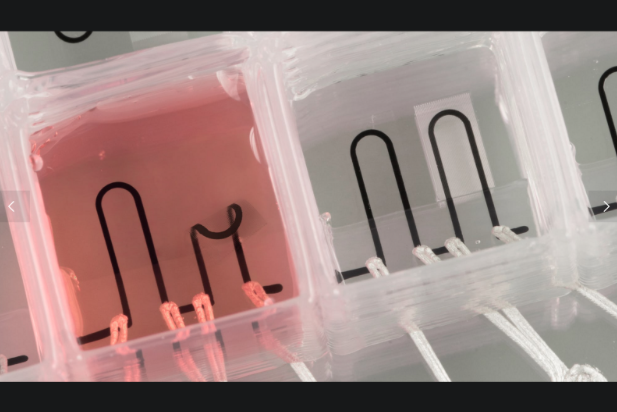
In 2016 the Wyss Institute in cooperation with SEAS managed to build in sensors into the structure of a 3D bioprinted OOC for the first time in the history. This achievement is important, because not only can they now customise the OOC, but the mechanical data, physiological parameters and drug absorption acquisition is significantly better.
This microchip contains different isolated wells that have multiple types of cardiac cells in it. It allows the researchers to study the behaviour and physiology of the different cell types in one experiment – significantly reduce the turnaround time and cost of the research by increasing the throughput of the technology.
Wyss Institute was always among the leaders in OOC research. Nothing demonstrates the elegance of their work more so than what they achieved with their Design of The Year prize in 2015 by the Museum of Modern Art.
This small device is a minor miracle – an incredible engineering achievement. Geraldine Hamilton, one developer of the OOC technology from Wyss, and CSO of Emulate has spoken about how to transform body parts into a small chip. Her talk was originally recorded in a TEDxBoston event in 2013. Since then an increasing amount of research has been presented to the community, but the fundamentals of their technology is summarized in an excellent way – in only 13 minutes :).
As Geraldine explains it is relatively easy to suggest new small molecule drug technologies, but the hard part is testing them. Organs-on-chips technologies can bring research to a new horizon. With their capacity it is possible to test the response and delivery of different drugs, not only for one, but even more types of cells and organs as well. Not only are they able to reduce the cost of drug delivery research and increase the throughput of the studies, but OOC’s also offer an alternative approach to replace animal studies.
Of further interest is that OOC has the possibility to be fully personalised. Following the whispers of big believers and sci-fi fans, we can imagine and hope that the day will come when patients will just walk into the doctor’s office and they will have the possibility to test the efficiency and response of the drugs they are meant to receive on their own cells.
But let’s not get ahead of ourselves just yet… The age of body-on-a-chip has not come yet. Scientists are working to integrate multiple types of cell into one chip to mimic the whole body in one device, but this work is in progress.
Another pioneer, MIT, runs different projects to work on the integrated body-on-a-chip project. Just recently they managed to come up with a new technique that can create pancreatic cells on the surface of a chip by differentiating stem cells into pancreatic beta cells on demand.
Professor Ron Weiss at MIT who leads the research has talked about the dream that one day this technique, growing organs from stem cells, can shorten the waiting time of the patients who needs life saving transplants. As we wait for this time to come the good news is that we can use this technology almost immediately to test drugs on human tissue.
OOC is a fantastic technology that is currently emerging. What will it bring to medicine? Personalised high-throughput and more reliable drug tests and a reliable validation method – and hopefully one day it will enter to the transplantation medicine as well. We are looking forward to it!
To stay tuned with additional reading, we recommend some pages to follow if one is interested in OOC research:
Wyss Institute from Harward University
Harward SEAS
MIT News
Nature
Emulate
Written by Fruzsina Félegyházi, Technical Writer